Contents
What is supraventricular tachycardia (SVT)?
Supraventricular tachycardia (SVT) is a type of heart rhythm disorder (arrhythmia) that originates in the upper chambers of the heart, known as the atria. The main symptom of SVT is a rapid heartbeat.
A normal adult heart rate ranges between 60–100 beats per minute (BPM). In SVT, the heart rate exceeds 100 BPM and may even reach 220 BPM or higher.
Here are several types of SVT:
- AVNRT (Atrioventricular Nodal Reentrant Tachycardia): The most common form of SVT, caused by electrical signals looping through the AV node twice.
- Atrioventricular reciprocating tachycardia (AVRT): Occurs when there’s an extra electrical connection between the upper and lower chambers, causing impulses to travel more quickly.
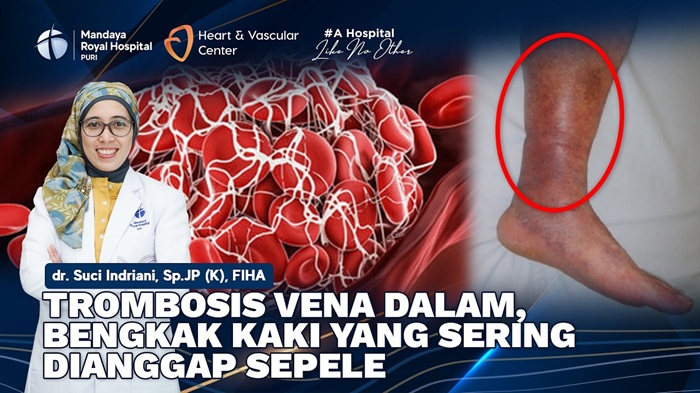
- Atrial fibrillation: In this condition, the atria beat irregularly and rapidly, increasing the risk of blood clots and stroke.
- Atrial flutter (AFL): In AFL, the atria can beat very fast (up to 300 BPM), although the ventricles typically follow a regular and slower conduction pattern.
- Paroxysmal SVT: SVT episodes that occur intermittently and often stop on their own.
- Atrial tachycardia: This form occurs when the electrical signals originate from somewhere in the atria other than the sinoatrial (SA) node.
Symptoms of SVT
The symptoms of SVT vary depending on how fast the heart is beating. They may include:
- Heart palpitations
- Dizziness
- Sweating
- Shortness of breath
- Chest pain
- Fainting
Causes of SVT
SVT is caused by disturbances in the heart’s electrical signals. These signals are responsible for controlling the heartbeat. In SVT, changes in these signals cause the heartbeat to begin prematurely in the upper chambers of the heart. When this happens, the heart beats faster and does not fill with blood properly. As a result, symptoms such as dizziness or lightheadedness can occur.
To understand the causes of SVT, it’s important to know how the heart normally functions.
The heart has four chambers:
- Two upper chambers called atria
- Two lower chambers called ventricles
In the upper right chamber is a group of cells called the sinus node, which generates the signals that initiate each heartbeat. The signal travels across the atria and reaches a group of cells called the AV node, where it usually slows down before continuing to the lower chambers.
In a healthy heart, this signaling process works smoothly, and the heart typically beats 60–100 times per minute at rest. In SVT, the heart beats faster—ranging from 150 to 220 BPM.
Diagnosing SVT
Several tests may be recommended by your doctor to diagnose SVT:
- Electrocardiogram (ECG/EKG): If SVT is suspected, your doctor may order an EKG. During this test, electrodes are placed on the chest to detect the heart’s electrical activity and produce a printed reading.
- Holter monitor: A portable EKG device that can be worn at home for 1–2 days to record continuous heart activity. It helps detect irregular rhythms that might not appear during a standard EKG.
- Echocardiogram: Uses sound waves to create images of the heart’s activity. It shows how blood flows through the heart and its valves.
Treatment for Supraventricular Tachycardia (SVT)
Hospital treatment may be necessary if SVT episodes are prolonged.
Treatment options include:
- Medications to control SVT episodes (administered as tablets or intravenous infusions)
- Cardioversion, a procedure that delivers small electric shocks to the heart to restore normal rhythm
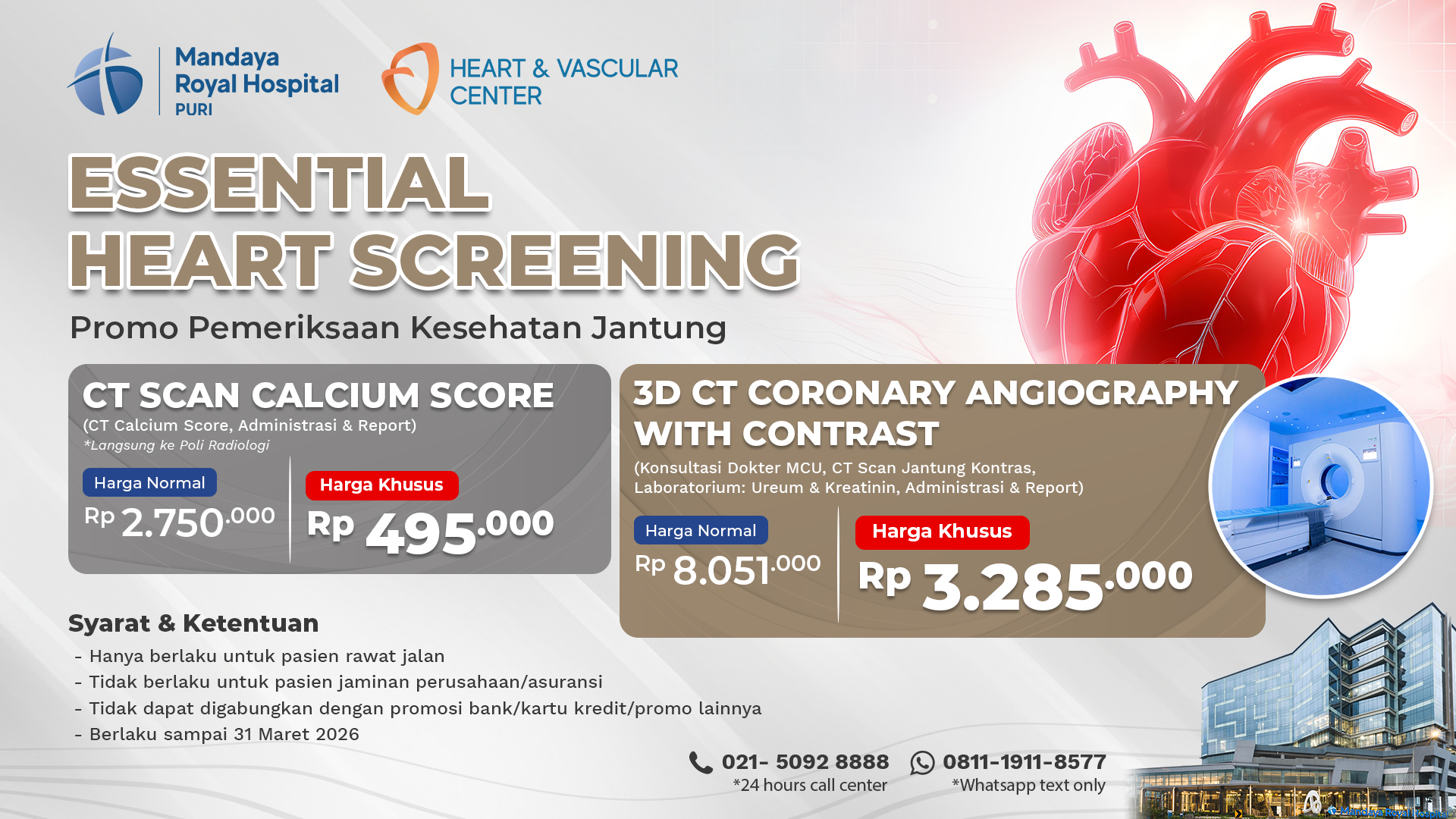
If you have more questions about SVT, don’t hesitate to visit Mandaya Royal Hospital Puri. Our hospital is equipped with modern, advanced medical technology and supported by a team of experienced specialists.
Use the Chat via WhatsApp, Book Appointment, or the Care Dokter app—available on Google Play and the App Store—for easier visits, queue tracking, and complete information.
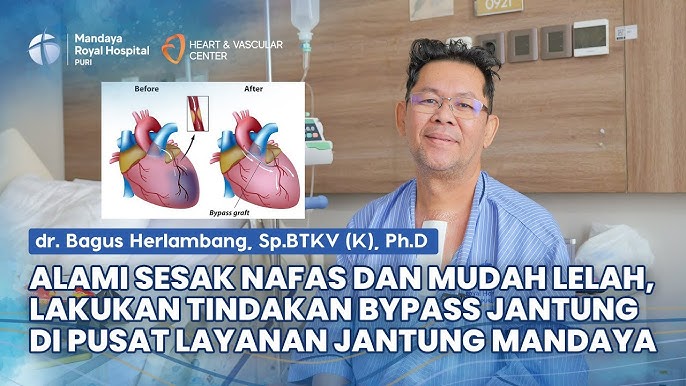
Arrhythmia Treatment at Mandaya Royal Hospital Puri
Mandaya Royal Hospital Puri offers a variety of treatments for arrhythmias such as SVT, including:
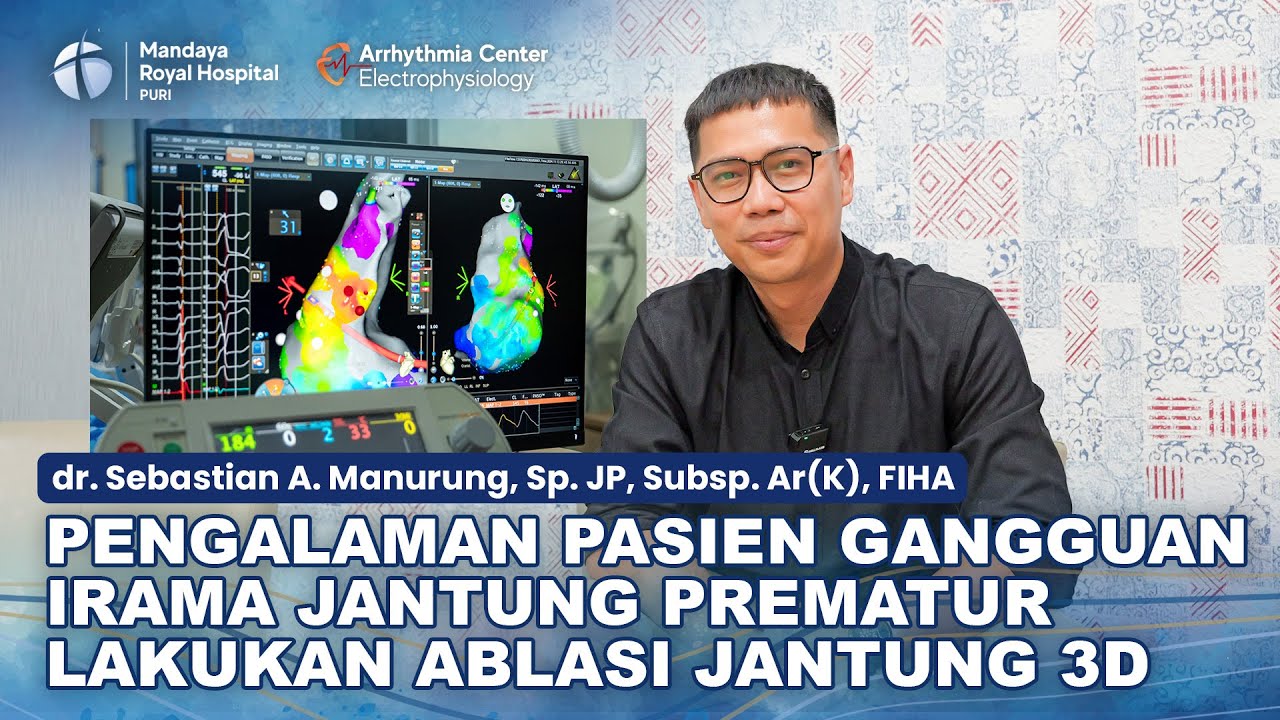
2D & 3D Cardiac Ablation
The hospital provides 2D and 3D cardiac ablation procedures using heat or cold energy to treat arrhythmias. During this procedure, a catheter is inserted into the patient’s heart to deliver thermal or cryoenergy that “scars” the heart tissue. These scars block the abnormal electrical signals that cause irregular heartbeats.
Key differences between 2D and 3D cardiac ablation:
- 2D ablation uses conventional mapping with fluoroscopy
- 3D ablation provides more detailed mapping technology
- 2D mapping identifies hundreds to thousands of points
- 3D mapping generates tens of thousands of data points, providing a much clearer heart image
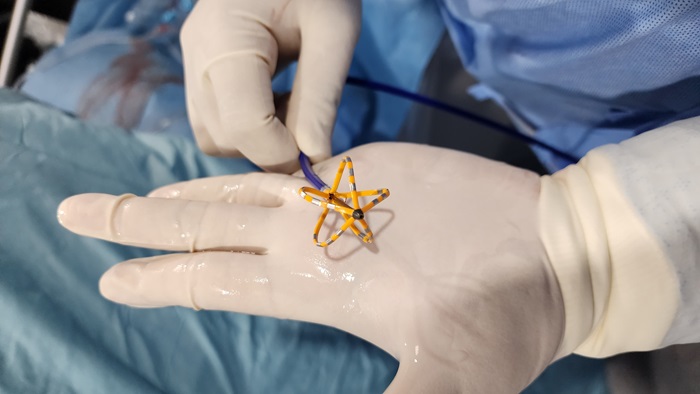
Pulse Field Ablation (PFA)
Unlike 2D and 3D ablation, which use single-point catheters, PFA uses multipolar or multipoint catheters that can deliver energy to multiple areas simultaneously.
PFA doesn’t use heat or cold energy but delivers strong electric pulses to repair damaged areas of the heart—typically used to treat atrial fibrillation.
Both 2D & 3D ablation and PFA procedures at Mandaya Royal Hospital Puri are performed by Dr. Sebastian Andy Manurung, Sp.JP, Subsp.Ar(K), FIHA, a Cardiology and Arrhythmia Consultant.