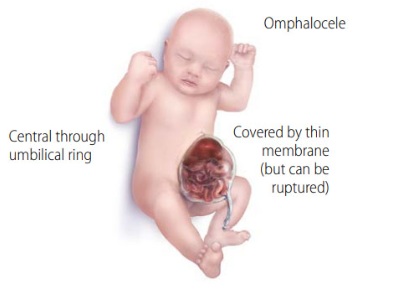
Omphalocele is a congenital birth defect where a baby’s abdominal organs protrude through an opening near the navel. These organs are covered by a thin, transparent sac made of peritoneum.
Omphalocele develops in the womb before the baby is born. At 6–10 weeks of pregnancy, the fetal intestines normally extend into the umbilical cord as part of the natural growth process. However, by the 11th week, the intestines should return to the abdominal cavity. If this does not happen, an omphalocele forms.
More than two-thirds of babies with omphalocele also have other abnormalities in the spine, digestive system, heart, urinary system, or limbs.
Contents
Types of Omphalocele
-
Small Omphalocele
A small omphalocele occurs when part of the intestines protrudes outside the abdomen through the navel. The defect usually measures less than 5 cm.
-
Large Omphalocele
A large omphalocele occurs when most abdominal organs—including the intestines, liver, and spleen—protrude outside the abdomen. This condition is larger than 5 cm and is often referred to by medical professionals as a giant omphalocele.
Causes of Omphalocele
Between weeks 6 and 10 of pregnancy, it is normal for the fetal intestines to extend into the umbilical cord as part of development. However, by week 11, the intestines should return to the abdominal cavity. If this does not occur, an omphalocele develops.
The exact cause of why some babies develop omphalocele while others do not is still unknown. Currently, there are no confirmed steps that can be taken during pregnancy to prevent this condition.
Risk Factors of Omphalocele
Research continues to identify risk factors that may increase the chance of a baby being born with omphalocele. Some possible factors include:
- Maternal age over 35 years.
- Alcohol consumption during pregnancy.
- Exposure to certain chemicals or toxins, such as pesticides or solvents.
- Genetic factors, as omphalocele can sometimes run in families. It is also associated with chromosomal abnormalities such as Trisomy 13, Trisomy 18, and Trisomy 21 (Down syndrome).
- Maternal health conditions such as obesity, diabetes, or hypertension.
- Nutritional or vitamin deficiencies during pregnancy.
- Smoking habits.
- Use of certain medications during pregnancy, such as selective serotonin reuptake inhibitors (SSRIs) or fertility drugs, which may increase the risk of omphalocele.
Symptoms of Omphalocele
Symptoms of omphalocele may include:
- A bulge at the navel covered by a thin, transparent membrane.
- Abdominal organs (such as intestines, liver, or spleen) visibly protruding outside through an opening in the abdominal wall.
- An unusual or abnormal-looking belly button.
- In large omphalocele, most abdominal organs are outside the body.
- Often accompanied by other congenital defects, such as heart, spine, digestive, or chromosomal abnormalities.
Diagnosis of Omphalocele
Omphalocele is usually diagnosed during the second or third trimester through prenatal ultrasound. Ultrasound allows doctors to see the baby’s organs developing outside the abdominal wall. If detected, doctors may also perform a fetal echocardiogram (fetal heart ultrasound) to check for heart abnormalities.
In some cases, omphalocele is not detected during pregnancy and only becomes apparent immediately after birth. The medical team will act quickly to protect the newborn’s health.
If a fetus is diagnosed with omphalocele, additional tests may be needed during the rest of the pregnancy, such as:
- Amniocentesis: A procedure to take amniotic fluid for testing chromosomal abnormalities.
- Blood test: Measuring maternal alpha-fetoprotein (AFP) levels. High AFP may indicate the need for further evaluation.
- MRI (Magnetic Resonance Imaging): To assess the baby’s heart, lungs, and other organs.
- Serial ultrasounds: Regular scans to monitor fetal growth.
After birth, doctors will examine the omphalocele directly and may run additional tests if necessary.
Treatment for Omphalocele
Treatment depends on factors such as gestational age at birth, the baby’s overall health, the severity of omphalocele, the size of the defect, and whether the organs are still protected by the membrane.
-
Treatment for Small Omphalocele
In small cases, surgery is usually performed shortly after birth. The goal is to return the protruding organs into the abdomen and close the abdominal wall opening to prevent infection and tissue damage.
-
Treatment for Large Omphalocele
For large omphalocele involving multiple organs, surgery is typically performed in stages. Surgeons gradually move the organs back into the abdomen over days to weeks. During this process, the organs are covered with a sterile sheet to prevent infection.
This staged approach is considered the safest method. In babies with large omphalocele, the abdominal cavity is too small and underdeveloped to accommodate all the organs at once. Immediate closure may also cut off blood supply to the organs. By waiting, the abdominal cavity has time to expand. Most babies undergo additional surgery within two weeks to restore normal anatomy.
Surgeons may also need to stretch the abdominal skin to close the defect. In some cases, a skin flap procedure—moving tissue from one body part to another—is necessary.
Babies with large omphalocele and underdeveloped abdominal cavities often have breathing difficulties. They may require ventilator support until they can breathe independently.
dr. Sastiono, Sp.B Subsp.Ped(K) – Pediatric Surgeon at Mandaya Royal Hospital Puri

Mandaya Royal Hospital Puri is home to one of Indonesia’s leading pediatric surgeons, dr. Sastiono, Sp.B Subsp.Ped(K). He is highly experienced in treating rare and complex pediatric cases that require surgery.
dr. Sastiono completed his medical education at the Faculty of Medicine, Universitas Indonesia (FK UI), including specialist and subspecialist training, and earned the title of Pediatric Surgery Consultant at FK UI. His expertise is widely recognized, especially in pediatric liver transplantation and hepatobiliary surgery involving the liver, gallbladder, bile ducts, and pancreas.
In addition to managing omphalocele, dr. Sastiono has extensive experience in pediatric surgery for various conditions, including:
- Biliary atresia in infants (bile duct blockage).
- Anal atresia (congenital absence or malformation of the anus).
- Hernia in children.
- Appendicitis in children.
- Intestinal obstruction in children.
- Various pediatric liver diseases.
- Hirschsprung’s Disease.
With his vast experience and expertise, Dr. Sastiono is a trusted referral for parents seeking safe and professional pediatric surgery.
Clinic Schedule – Dr. Sastiono, Sp.B Subsp.Ped(K):
- Tuesday: 10.00 – 13.00 WIB
- Thursday: 10.00 – 13.00 WIB
To consult with Dr. Sastiono at Mandaya Royal Hospital Puri, you can visit directly or use the hospital’s convenient services such as WhatsApp Chat, Book Appointment, or the Care Dokter app available on Google Play and the App Store for appointment booking, queue numbers, and complete information.



