Facial twitching, medically known as hemifacial spasm, is a neurological condition that causes involuntary and repetitive contractions of the facial muscles. Although it may appear mild, this condition can interfere with daily activities, reduce self-confidence, and significantly affect a patient’s quality of life. Today, facial twitching can be treated through Microvascular Decompression (MVD) surgery performed by Dr. dr. Mardjono Tjahjadi, Sp.BS, Subsp. N-Vas, F. N-Onk, PhD, FICS, IFAANS (Dr. Joy) at Mandaya Royal Puri Hospital, offering a medical solution that directly addresses the underlying cause of hemifacial spasm.
Contents
Understanding MVD for Treating Facial Twitching
MVD is a surgical procedure aimed at relieving pain or muscle twitching caused by pressure from blood vessels—either arteries or veins—on a nerve. This procedure involves opening a small portion of the skull so the doctor can directly visualize the nerve at the base of the brainstem.
Next, the surgeon places a special pad or sponge between the nerve and the compressing blood vessel, protecting the nerve from pulsation and pressure. With this technique, symptoms caused by nerve compression can be significantly reduced.
In MVD procedures, the pad is typically placed between the trigeminal nerve and the superior cerebellar artery or branches of the petrosal vein that are causing the compression. Once the pressure on the nerve is relieved, symptoms such as pain or twitching may subside, leading to improved quality of life.
How Is the MVD Procedure Performed?
Below are the stages before, during, and after MVD surgery performed to treat facial twitching:
1. Preoperative Stage
Before undergoing MVD, patients will go through a series of medical examinations to ensure their condition is stable and safe for major surgery under general anesthesia. After the anesthesia takes effect and the patient is asleep, a small area of hair behind the ear on the affected side will be shaved, approximately 2.5 x 7.5 cm in size. The patient’s head is then positioned carefully and secured with special equipment to keep it stable throughout the procedure.
2. Intraoperative Stage
Once the head is optimally positioned, the neurosurgeon creates a small opening in the skull behind the ear, usually about the size of a coin. The protective layer of the brain (dura) is then opened to access the nerve. Using an operating microscope, the surgeon identifies the cranial nerves, particularly the root of the trigeminal nerve connected to the brainstem (pons). In this area, arteries or veins are often found compressing the nerve and causing symptoms.
During the procedure, other medical specialists such as neurologists or neurophysiologists monitor auditory nerve function using specialized equipment. This monitoring is essential because the auditory nerve pathway is close to the surgical area and must be carefully protected.
3. Postoperative Stage
After the MVD procedure is completed, the patient is transferred to the recovery room for monitoring of vital signs until the effects of anesthesia fully wear off. The patient is then typically admitted to the ICU for one night for close observation. During the early recovery phase, symptoms such as nausea or headache may occur, but these are generally manageable with medication.
Once the patient’s condition is stable, care continues in a regular inpatient room. Patients are gradually encouraged to perform light activities, such as sitting up or walking slowly. In many cases, patients are able to go home within 1–2 days after surgery, with detailed instructions for follow-up care at home.
Profile and Expertise of Dr. Joy, Neurosurgeon Specialized in MVD
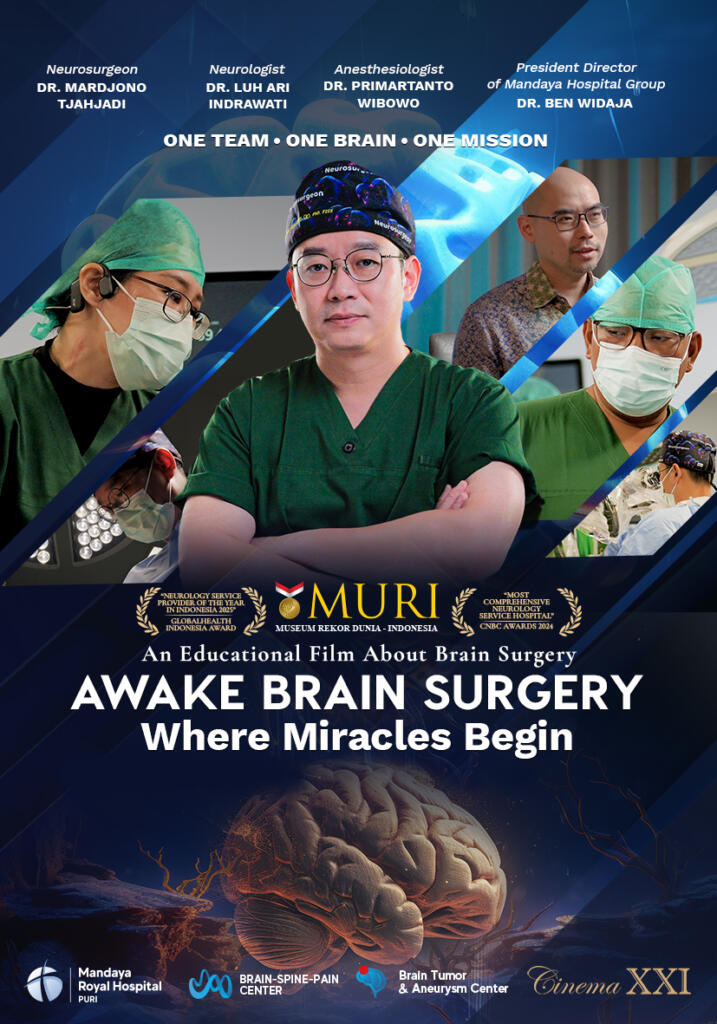
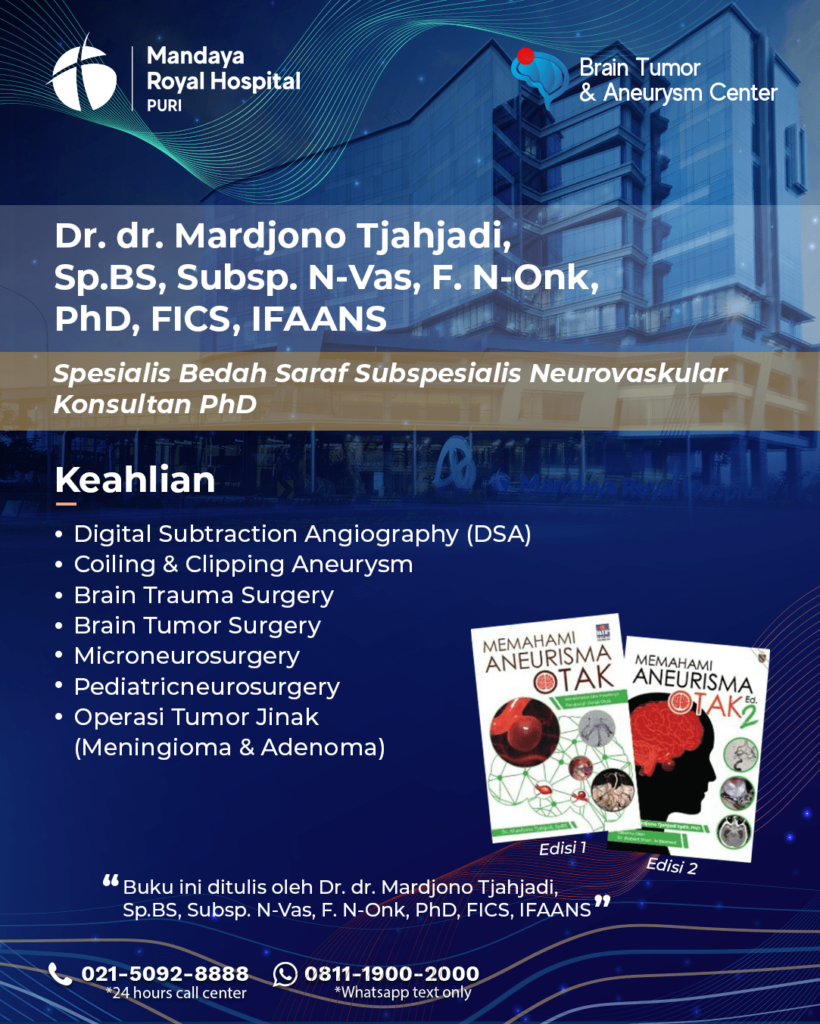

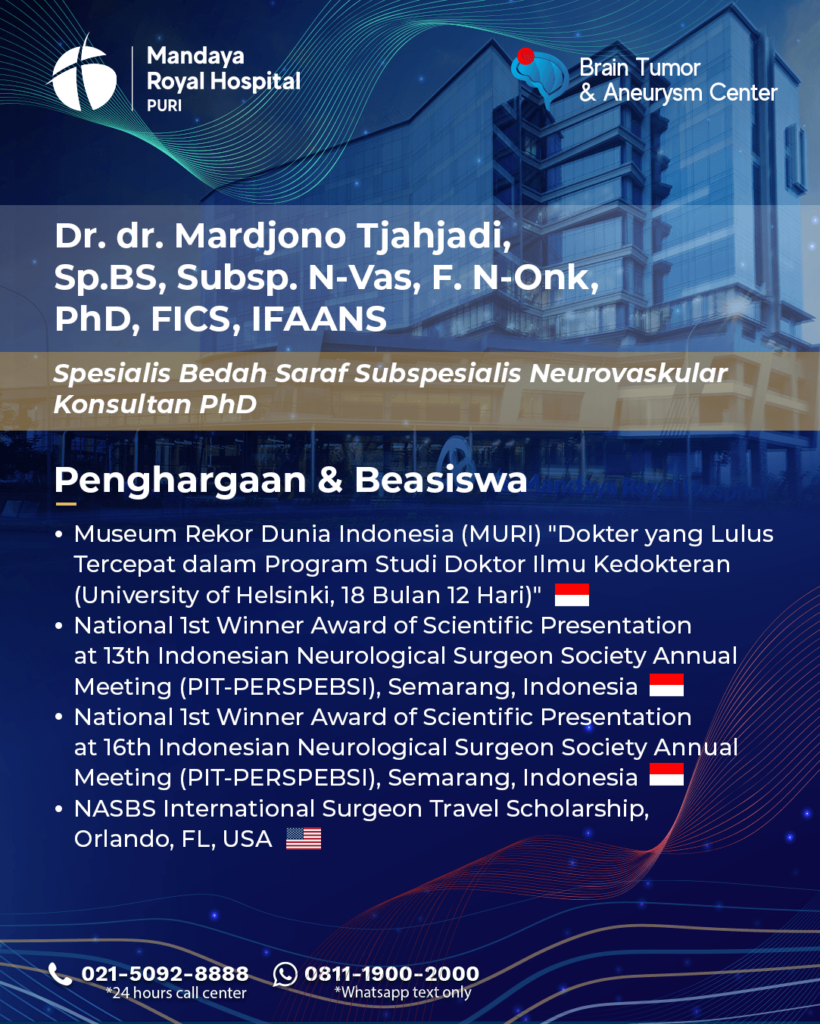
Dr. dr. Mardjono Tjahjadi, Sp.BS, Subsp. N-Vas, F.N-Onk, PhD, FICS, IFAANS, widely known as Dr. Joy, began his medical education at one of Indonesia’s leading universities. Since his early academic years, he has shown a strong interest in neurosurgery, particularly in the neurovascular subspecialty. After completing his medical education in Indonesia, Dr. Joy pursued his neurosurgical specialist training in Finland, where he studied directly under world-renowned neurosurgeons and actively participated in cutting-edge research on aneurysms and brain tumors.
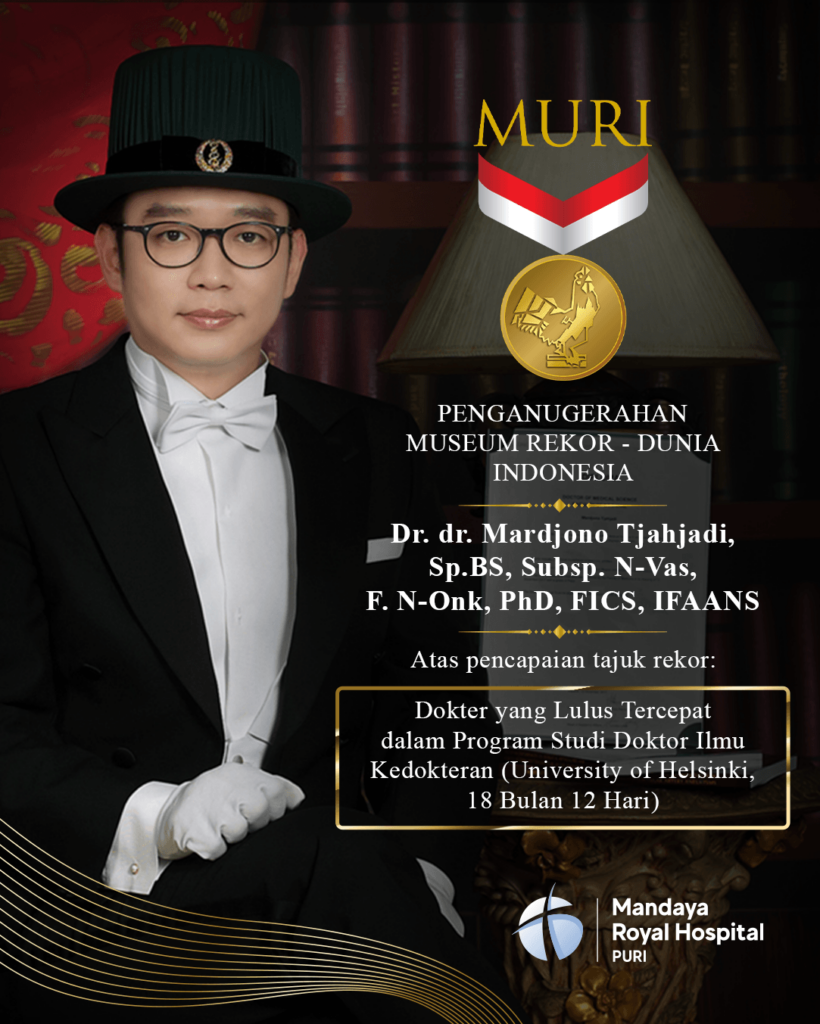
Dr. Joy’s academic excellence became even more prominent when he completed his doctoral (PhD) program in Finland in an exceptionally short time—only 18 months and 12 days. This remarkable achievement earned him an award from the Indonesian World Records Museum (MURI) as the “Fastest Doctor to Complete a Medical PhD.”
Today, Dr. Joy is widely recognized as one of Indonesia’s leading neurosurgery specialists, with extensive experience in managing complex neurological cases. His expertise includes the treatment of brain aneurysms, brain hemorrhages, brain tumors, and brain cancer, using a comprehensive, technology-driven medical approach. Supported by strong academic credentials and international experience, Dr. Joy has received numerous awards and recognitions at both national and international levels.
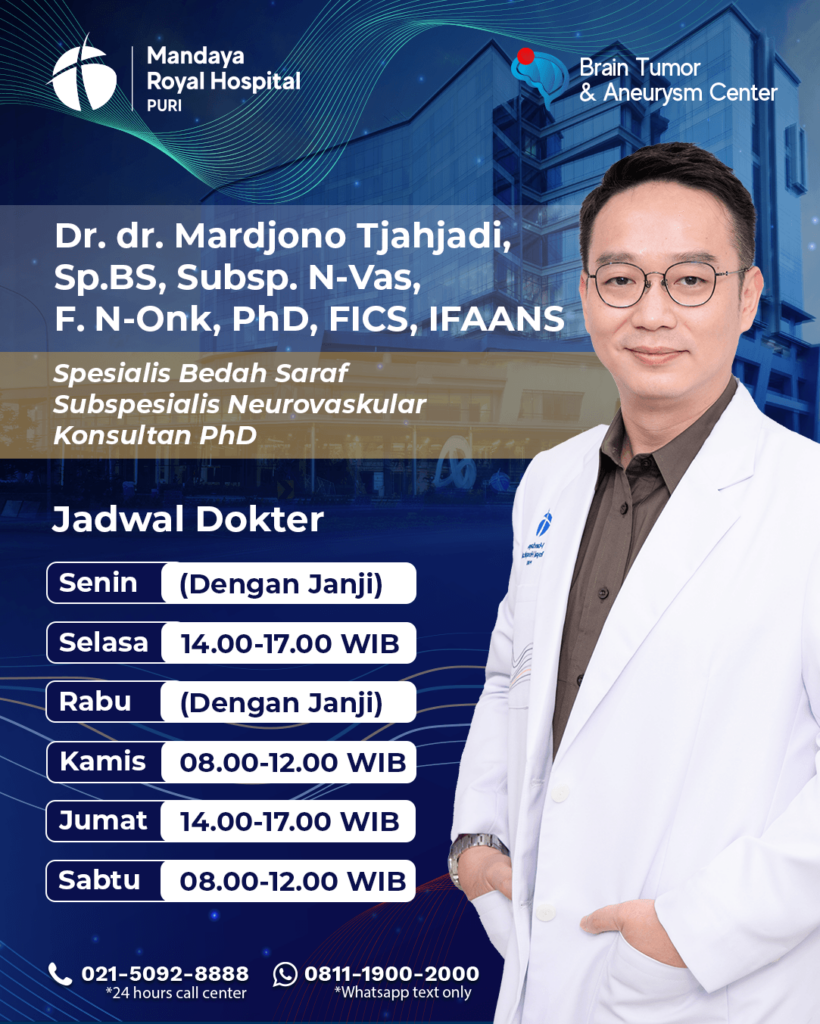
Dr. Joy’s Practice Schedule at Mandaya Royal Puri Hospital
The practice schedule of Dr. dr. Mardjono Tjahjadi, Sp.BS, Subsp. N-Vas, F. N-Onk, PhD, FICS, IFAANS at Mandaya Royal Puri Hospital is as follows:
- Monday: by appointment
- Tuesday: 2:00 PM – 5:00 PM
- Wednesday: by appointment
- Thursday: 8:00 AM – 12:00 PM
- Friday: 2:00 PM – 5:00 PM
- Saturday: 8:00 AM – 12:00 PM
To make your visit easier, please use the WhatsApp Chat feature, Book Appointment, or the Care Dokter application, available for download on Google Play and the App Store, to schedule visits, view queue numbers, and access complete information.



