Peripheral artery disease (PAD) is a condition where arteries in the legs, pelvic area, or arms become narrowed or blocked, most often due to plaque buildup. This blockage disrupts blood flow and can cause symptoms such as leg pain. The good news is that PAD is treatable, especially when diagnosed early.
PAD is common, affecting around 200 million people worldwide. Anyone can develop the condition, but the risk increases with age.
Contents
Causes of Peripheral Artery Disease
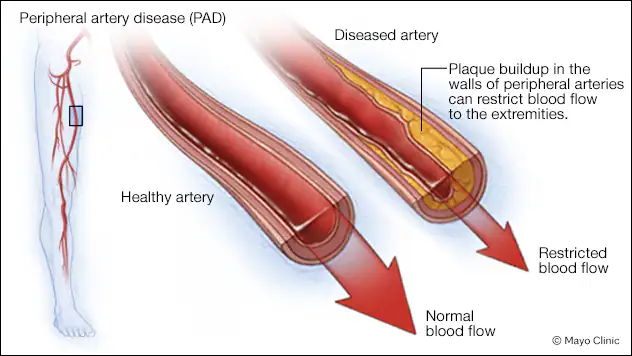
The most common cause of PAD is gradual plaque buildup inside the arteries, a condition known as atherosclerosis. Arteries are hollow tubes with smooth inner walls that help prevent clotting and ensure steady blood flow. In PAD, plaque slowly develops along the artery walls, narrowing the passage for blood flow.
Plaque is typically hard on the outside and soft on the inside. The hard surface can crack, causing platelets (disc-shaped blood cells that help clotting) to stick to the site. This may result in blood clots that narrow the artery further.
If plaque or blood clots significantly narrow or block the artery, blood flow cannot reach tissues downstream of the blockage. This often happens in the toes and feet, leading to tissue damage or death.
Although atherosclerosis is the main cause, PAD can also be caused by rarer conditions such as vasculitis (artery inflammation) or Popliteal Artery Entrapment Syndrome (PAES), where repeated pressure on the artery behind the knee restricts blood flow.
Risk Factors for PAD
You are at higher risk of developing PAD if you have:
- A history of smoking (past or current)
- Chronic kidney disease
- Diabetes
- High blood pressure
- High cholesterol or triglycerides
Studies show that smoking and diabetes are the strongest risk factors for PAD. People in these groups are 2–4 times more likely to develop the disease compared to those who do not smoke or have diabetes.
If you have coronary artery disease or multiple atherosclerosis risk factors, your doctor may recommend PAD screening tests to detect the condition early.
Symptoms of Peripheral Artery Disease
The earliest and most common symptom of PAD is discomfort in the legs during physical activity. This occurs because narrowed arteries cannot supply the increased blood needed by the muscles. As the disease progresses, pain may even appear when resting. However, many people experience no symptoms and only discover PAD through screening.
Possible symptoms include:
- Leg discomfort during activity: Pain, cramping, numbness, or fatigue in the calves, thighs, or buttocks when walking or climbing stairs. Symptoms usually subside within 10 minutes after stopping.
- Rest pain: As PAD worsens, dull or burning pain may develop in the legs, feet, or toes, especially when lying down. Pain may ease when the legs are dangled off the bed.
- Non-healing wounds: Sores on the feet or toes that do not heal and may become infected.
- Skin color or temperature changes: Blocked arteries can cause skin to turn purple, green, black, or very pale. Skin may feel cold or tingly. These are signs of severe PAD that require urgent medical care.
Symptoms depend on which artery is affected:
- Buttock, hip, or thigh discomfort: narrowing of the lower aorta or iliac arteries (pelvic area).
- Calf discomfort: narrowing of the femoral or popliteal arteries (thigh or knee area).
Men with narrowing in the lower aorta or iliac arteries may also experience erectile dysfunction linked to PAD.
Complications of PAD
Without proper treatment, PAD may lead to limb loss (amputation). Fortunately, most PAD patients do not reach this stage, as doctors work to prevent it. But if tissue damage is severe or life-threatening, amputation of toes, feet, or part of the leg may be necessary.
PAD patients are also more likely to have coronary artery disease and cerebrovascular disease. While not direct complications of PAD, these conditions often occur together since plaque buildup usually affects multiple arteries, not just those in the legs.
Treatment for Peripheral Artery Disease
Treatment depends on the severity of the condition. For mild or asymptomatic cases, lifestyle changes and medication may be enough. In advanced cases, medical procedures or surgery may be required.
1. Medications for PAD
- Blood thinners: Reduce the risk of clots. Doctors may prescribe antiplatelets such as clopidogrel or aspirin, or low-dose rivaroxaban in some cases.
- Vasodilators: Help widen blood vessels to improve circulation and reduce leg pain, such as cilostazol.
- Statins: Lower LDL cholesterol to protect against amputation and cardiovascular death.
- Blood pressure medications: Reduce the risk of heart attack, stroke, heart failure, and death.
- Smoking cessation aids: For PAD patients who smoke, quitting is crucial to reduce complications and prevent limb loss.
2. Foot Care for PAD Patients
Since PAD reduces blood flow, proper foot care is critical:
- Check feet daily for cracks or wounds
- Wash and dry feet daily
- Avoid walking barefoot
- Wear comfortable, well-fitting socks and shoes
3. Procedures and Surgery
If PAD is severe or does not improve with medication, the following procedures may be recommended:
- Angioplasty: A small balloon is inflated inside the artery to push plaque aside, sometimes with a stent to keep it open.
- Atherectomy: A catheter is used to remove plaque from the artery.
- Endarterectomy: Surgical removal of plaque from the artery.
- Peripheral artery bypass surgery: A new pathway is created to reroute blood around the blocked artery.
When to See a Doctor
Seek medical care if you experience:
- New or worsening symptoms
- Difficulty walking that affects daily life
- Leg pain at rest
- Wounds or ulcers on the feet or toes
If you are at risk of PAD but have no symptoms, consult your doctor for early screening. Early detection and treatment can prevent amputations and save lives.
Go to the Emergency Department immediately if you cannot move or feel your leg, or if one leg looks different in color from the other. This may signal a sudden loss of blood flow requiring urgent care.
PAD Treatment for Diabetic Foot at RS Mandaya Royal Puri
RS Mandaya Royal Puri has a cardiovascular specialist and consultant in interventional and vascular cardiology experienced in treating PAD through revascularization with plaque debulking (plaque “drilling”). She is dr. Suci Indriani, Sp.JP (K), FIHA.
According to dr. Suci, PAD treatment is similar to procedures performed on the heart. When arteries are blocked, blood flow must be restored to ensure proper circulation.
The procedure is minimally invasive, performed with a catheter rather than open surgery, typically through the femoral artery (groin). The first step is angiography to visualize the arteries and confirm blockages. Based on results, treatment may include balloon angioplasty, stent placement, clot aspiration, or specialized plaque removal devices.
Not all cases require stent placement—the main goal is restoring blood flow to the legs so oxygen and nutrients can reach the tissues, preserving limb health.

dr. Suci Indriani’s Practice Schedule at RS Mandaya Royal Puri
- Monday: 17.00 – 20.00
- Friday: 17.00 – 20.00
For convenient access, use the Chat via WhatsApp, Book Appointment, or download the Care Dokter App from Google Play and App Store to schedule visits, check queue numbers, and get complete information.



